An internet friend with ME, has mailed me his response to the BMJ NICE editorial. It was rejected, or should I say, not placed. Why? Well that is quite easy. He used to be a happy, sporty, good looking guy he assures me, until he was struck down by ME. But to make matters worse, he also has a name that people keep making fun off. If you see him or mail him, please don’t do this, as he is sick and tired of hearing the same joke over and over again. What is his name? Simon Wessely. Not the CBT delusional fanatic, but a normal, likeable GP, who is now dependant on his elderly parents and carers. If you want to cheer him up, you can reach him at: simonwessely@yahoo.com
I will place his response below, as I can't see any words in it that would be offensive or so. Far from it. Another sign that the BMJ is not unbiased at all. See for yourself.
"THE (ME) WORLD ACCORDING TO NICE:
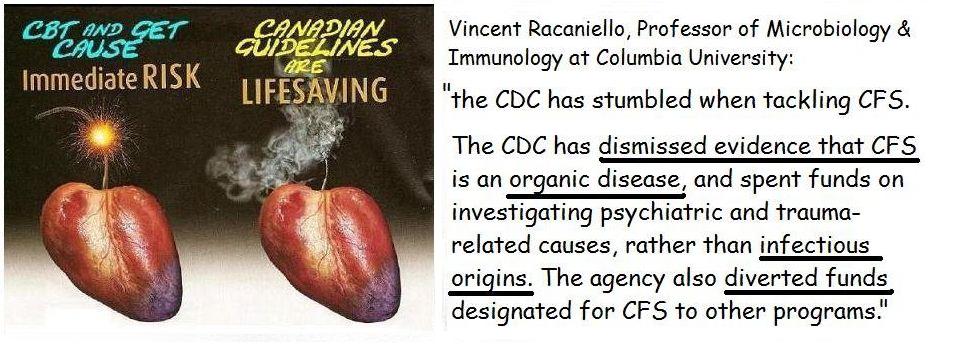
Why is it that GET (Graded Exercise Therapy) is mentioned but has no one at Nice heard about the threshold phenomenon? When I was fit and well I could train and improve my stamina by increasing my training with a maximum of 10% a week, so I wouldn't get injured and I completed a marathon in just over three hours. And I have kept fit my whole life, just because I like sport. The trouble with ME is that you can’t increase your stamina. My body tells me exactly what the threshold is. And the only one who can change this is my body. I have seen some other symptoms decrease or disappear and I hope the same will happen to this threshold. Obviously I have tried the same principles I used in running to increase my threshold since I have ME, but every time I do so, things get a lot worse. At the moment I can manage to walk the enormous distance to the toilet and back. But only once an hour. If I do it twice, a one hundred percent increase, the pain is so extreme, that even a piece of paper on my legs hurts a h… of a lot. GET is a very quick way though to know if someone has ME. If they can train and improve, they don’t have ME. The trouble though is, that it is very easy to get a relapse due to GET, and get a lot worse. So GET is NOT a good idea if you really have ME. I welcome advice by an institute as NICE about a disease. However, there are too many guidelines for busy GPs to read. The problem is, I’m having time, and my brain is starting to work again, so I can have a lookat these guidelines, even if this takes me days.
I’m one of those doctors with ME, and like many others I was taught that ME didn’t exist. So then to be diagnosed with ME was a bit of a shock to put it mildly. Before I fell ill, I have never been to my doctors but still, that didn’t mean that I was taken seriously. Interestingly enough one of them is a GP trainer, but even that didn’t help.
Reading your guideline all you need to have to diagnose ME is tiredness and a sore throat.
The Oxford criteria said: tiredness.
CDC/Fuduka said: tiredness plus a minimum of 4 out of 8 listed symptoms.
The Canadian and Australian Guidelines speak of a whole list of symptoms and it seemed that finally we were separating ME from other illnesses. And I’ll show you why this is important.
I have been confined to my bed for a long time with extreme muscle pains and cognitive dysfunction, such as difficulty with information processing. In reality this meant I could not read, use the laptop, listen to music or watch TV. As I couldn’t walk as well, I have had an interesting time, just like many others with this disease. Not to mention how GPs and others have perceived me and judged me. Now as a simple GP this sounds a bit different than tiredness and a sore throat. But I might be wrong.
You say in your guideline that “Most people with CFS/ME will improve over time and some will recover and be able to resume work and normal activities.” You also say “Offer cognitive behavioural therapy (CBT)” to help coping etc. This apparently is the best evidence based therapy as you call it. The interesting thing is, Nijmegen said in the Journal called: “Psychotherapy and Psychosomatics, Vol. 76, #3, pp 171-176, in April2007:
“After treatment, 69% of the patients no longer met the CDC criteriafor CFS.” So I would say as a simple GP, 69% was cured. Because if you meet the CDC criteria you have ME and once they are gone, you don’t have ME anymore. Their (Nijmegen) basis for CBT is: “Once the patient is convinced of the absence of a somatic cause for his symptoms, and is motivated to explore psychological consequences of his complaints (the first steps in CBT), he can benefit from CBT rapidly.”
In your guideline though, you say, advice CBT but only to cope, so it doesn’t cure. And that is exactly what the Canadians and Australians say in their guidelines; there is no cure for ME. So as a simple GP, what are we supposed to tell the patients, does CBT cure ME or not? And if it doesn’t cure, what every ME patient can tell you, then where is the evidence from all the Nijmegen articles, to use CBT in ME?
Interesting is also the fact that the WHO classifies ME as a neurological disease and I have always learned that psychosomatics was something else. But hey, wrong again. It gives a good idea though how people perceive a ME patient.
Also, if there is no cure for ME, it is even more important to make sure that we don’t label patients, who don’t have ME, as a patient with ME. For the simple fact, that we might be able to cure them. Sounds a lot better than no cure, I can assure you.
But from now on, many GPs will think, fatigue and sore throat = ME.
Another interesting thing in your guideline is the following statement: “The keys to pacing are knowing when to stop and rest by listening to and understanding one’s own body, taking a flexible approach and staying within one’s limits.” Nijmegen however states that we shouldn’t listen to our bodies because our illness beliefs are wrong. Once we overcome those, hoopla, ME gone.
If you however think that having ME is the worst part, then you are wrong. It is not only the extreme pains, the noise intolerance, for example simple noises like using cutlery to eat, or a door being shut, that makes too much noise, or a brain that doesn’t function. It is not only doctors, of the seven doctors in the practice, I have now found the one who actually thinks that someone who hasn’t been to the surgery for fifteen years, and then suddenly starts coming, might actually have a problem. Silly approach, I know.
It is also interesting to see how friends and family treat you and are calling you all sorts of names, because there is no test for ME. So we are lazy, not motivated because if we were motivated, we would have been better a long time ago. And you can think of a few other things people say. Some even do it every time they see you. Great. Is that what Nijmegen et al call the secondary gains of being ill? And I can assure you, going from sporty and very active, to a life in bed, is difficult enough to accept, let alone dealing with all those other things around ME. But if you read the comments here in the BMJ, for example those TV comments, then those are a hundred times more beneficial, than that hokus pokus CBT thing. I have tried it, as I want my normal life back, but I have never seen so much silliness being sold to me as therapy for ME. The other interesting thing about CBT is that if it works the psycho people have done a good job, and when it doesn’t it is my fault. A win win situation for Nijmegen et co. And what did we tell people with MS for decades, to name just one disease where we got it completely wrong? They had a catatonic unwillingness to move. False illness beliefs, interesting concept. But why don’t we learn from our mistakes in the past? And don’t forget, even you can get ME. Even if you think it is only for softies.
Competing interests: GP and ME patient, yes they do exist.”
And what does the BMJ say about themselve on their own website:
BMJ helping doctors make better decisions
Better decisions for whom though, is the question?
No comments:
Post a Comment