Frank N.M. Twisk 1 and Michael Maes 2:
Benign Myalgic Encephalomyelitis (ME) / Chronic Fatigue Syndrome (CFS) is a highly incapacitating illness classified by the WHO as a neurological disease (G93.3) since 1969 (WHO ICD-8, 1967).
The CFS Fukuda case definition (Fukuda et al. 1994), which has been has been criticized by several researchers, states that a CFS patient needs to experience chronic fatigue of new or definite onset, that is not substantially alleviated by rest, is not the result of ongoing exertion,
and results in substantial reductions in occupational, social, and personal activities. The Fukuda
case definition also requires the concurrent occurrence of at least four to eight other CFS symptoms, i.e. impaired memory or concentration, sore throat, tender lymph nodes, muscle pain, multiple joint pain, new headaches, unrefreshing sleep, and post-exertional malaise.
ME/CFS is considered to be a rather harmless condition by most physicians, but patients with ME/CFS are often more functionally impaired than those suffering from type 2 diabetes, congestive heart failure, multiple sclerosis, and end-stage renal disease (Anderson
& Ferrans, 1997; Buchwald et al. 1996).
Jason et al. (2006) analyzed a group of 166 individuals who had died with ME/CFS (listed at a US ME/CFS memorial register). The mean ages of the ME/CFS patients dying from heart failure (20,1%), cancer (19.4%), and suicide (20,1%) were 58.7, 47.8, and 39.3 years, respectively.
These ages are considerably lower than of those dying from heart failure (83.1 years), cancer (72.0 years), and suicide (48.0 years) in the general US population.
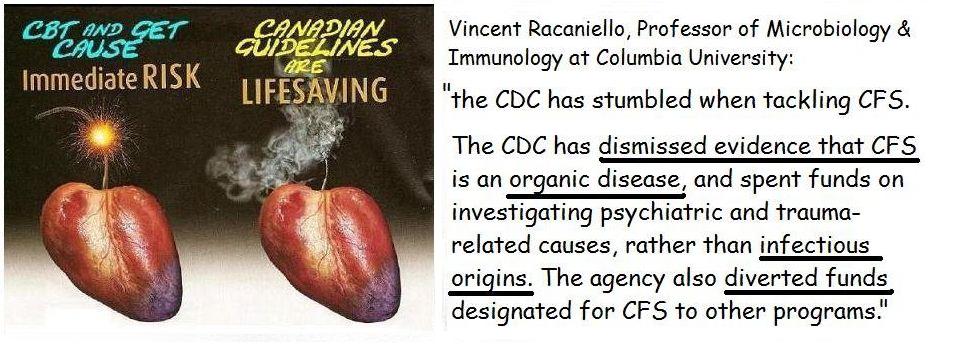
In spite of its chronicity and severity, ME/CFS remains highly controversial in the medical en political society. Despite several hundred studies demonstrating biological abnormalities in large subgroups, ME/CFS is still considered by many professionals to be a “medically unexplained syndrome” or a mental condition with a psychogenic/social origin. The psychosocial
explanatory model for “medically unexplained disorders”, disseminated by proponents of the (bio)psychosocial school, is the rationale for the combination of cognitive behavioral
therapy (CBT) and graded exercise therapy (GET), which are supposed to eliminate the psychogenic “maintaining factors” and “deconditioning”, respectively.
This review will show that:
a) the evidence-based success claim for CBT/GET is unjust, since the evidence base is lacking and CBT/ GET is not significantly more effective than usual care; and
b) the exertion, and thus GET, can have numerous potential damaging physical effects on ME/CFS patients.
PubMed
No comments:
Post a Comment